

It’s Endometriosis Awareness Month. Let’s Debunk 10 Myths About This Condition.
Summary
Endometriosis is not just a bad period; it’s a chronic condition with symptoms that extend beyond menstrual pain.It can affect more than just the reproductive organs, potentially impacting various parts of the body.
Pregnancy is not a cure for endometriosis; symptoms may improve during pregnancy but often return.
Endometriosis can be challenging to diagnose, as it’s not always visible on ultrasounds or MRIs.
It affects women of all ages, not just those in their 30s and 40s.
The severity of pain does not always correlate with the extent of the disease.
A hysterectomy is not a guaranteed cure; symptoms can persist if endometrial-like tissue exists outside the uterus.
Diagnosis can take time, often due to the similarity of symptoms to other conditions and lack of awareness.
Reflection Questions
- How do you prioritize self-care amidst managing endometriosis? Share the self-care practices that bring you comfort and strength, and explore any new practices you wish to incorporate into your routine.
- List the strategies that have helped you manage pain and discomfort. Which have been the most effective, and why do you think they work for you?
- Reflect on the treatments and therapies you’ve tried. What were your hopes for each, and how did the reality match up? Are there any new methods or approaches you’re curious to explore?
Journal Prompt
Consider the role of support systems in your journey. How have relationships with friends, family, or support groups impacted your experience with endometriosis?
March is Endometriosis Awareness Month, so we’re addressing a few myths and misconceptions about the women’s health condition. Endometriosis is very personal to us at DesignDash, as members of our team live with the chronic disease. If you have endometriosis or suspect that you might, we hope you receive the support, validation, and ongoing education necessary to feel in control, limit pain, reduce inflammation, and enjoy life. To learn more about endometriosis, please consult a specialist, seek out resources from reputable sources like the Endometriosis Foundation, and try not to get discouraged when you read misleading information. We hope this article helps you make sense of conflicting reports about endometriosis.
Debunking 10 Myths and Misconceptions About Endometriosis
#1 Endometriosis is Just Painful Periods
While painful menstruation (dysmenorrhea) is one of the most common symptoms of endometriosis, the condition entails much more than menstrual pain. Endometriosis is a chronic and often debilitating disease where tissue similar to the endometrium, the lining of the uterus, grows outside the uterus in areas like the pelvic cavity. This ectopic tissue behaves like the lining inside the uterus, thickening, breaking down, and bleeding with each menstrual cycle.
However, the blood and tissue shed from growths outside the uterus have no way to exit the body, leading to inflammation, pain, and the formation of scar tissue (adhesions). This process can cause chronic pelvic pain, not just during periods but also during intercourse, bowel movements, or urination. Moreover, endometriosis can lead to infertility in some endometriosis patients, with the inflammation and scar tissue affecting the ovaries, fallopian tubes, and the function of reproductive organs.
#2 It Only Affects the Reproductive Organs
While endometriosis is most commonly found on or around the organs of the pelvic cavity such as the ovaries, fallopian tubes, and the outer surface of the uterus, it is not confined to the reproductive organs. Endometrial-like tissue can be found in various locations throughout the body, including, but not limited to, the intestines, bladder, and rarely, in more distant organs such as the lungs or brain.
This widespread potential for endometrial-like tissue growth means that endometriosis can have systemic effects, potentially impacting gastrointestinal, urinary, and even respiratory function, depending on the location of the growths.
#3 Endometriosis is Always Visible on Ultrasounds or MRIs
Endometriosis poses significant diagnostic challenges. While ultrasound and MRI can be helpful tools in identifying endometriotic lesions, particularly larger ones or ovarian endometriomas (cysts filled with old blood), these imaging techniques may not detect smaller lesions or deeply infiltrating endometriosis.
The gold standard for diagnosing women with endometriosis is laparoscopy, a surgical procedure that allows direct visualization of the lesions, and often, their removal for biopsy. This method provides the most definitive diagnosis but is more invasive than imaging.
#4 Pregnancy Cures Endometriosis
The myth that pregnancy cures endometriosis likely stems from temporary symptom relief some women experience during pregnancy. Due to hormonal changes that suppress the menstrual cycle, such as elevated progesterone levels, some of the inflammation and pain associated with endometriosis can be alleviated. However, pregnancy does not eradicate the endometrial-like tissue outside the uterus, and symptoms may return after childbirth and the cessation of breastfeeding when normal menstrual cycles resume.
#5 Endometriosis is a Young Woman’s Disease
Endometriosis can affect anyone with a uterus, from their first menstruation until menopause. Symptoms may vary throughout a person’s life, particularly with changes in hormone levels, but the condition is not limited to young women. Older women, even those approaching menopause, can suffer from endometriosis. Symptoms might be misattributed to aging or other health conditions, delaying diagnosis.
#6 Hysterectomy Cures Endometriosis
While a hysterectomy (removal of the uterus) may alleviate symptoms for some individuals, particularly those for whom other treatments have failed, it does not guarantee a cure for endometriosis. Since endometriosis involves tissue similar to the lining of the uterus growing outside it, removing the uterus does not address lesions elsewhere in the body. Endometriosis is a complex condition that often requires a multifaceted treatment approach, including hormone therapy, pain management, and sometimes surgery to remove extensive endometriosis tissue.
#7 Endometriosis is Rare
Endometriosis is far from rare, affecting approximately 1 in 10 women and individuals assigned female at birth of reproductive age. This prevalence means that endometriosis is a common gynecological condition, yet it often goes undiagnosed or is misdiagnosed due to a lack of awareness and understanding among both the public and medical professionals. The normalization of menstrual pain and the variability of symptoms contribute to lack of adequate endometriosis diagnosis.
#8 Severe Pain is Normal for Menstrual Cycles
While mild to moderate discomfort can be a normal part of menstrual cycles, severe pain that disrupts daily life is not normal. Dysmenorrhea (painful periods) that significantly impacts one’s quality of life may be indicative of underlying conditions such as endometriosis.
Accepting severe pain as a normal aspect of menstruation can lead to delays in seeking treatment and diagnosis, prolonging suffering and potentially exacerbating the condition. It’s important for individuals to seek medical advice if they experience unusually painful periods or pelvic pain at other times of the cycle.
#9 Endometriosis is the Proliferation of Endometrial Tissue Beyond the Uterus
The belief that endometriosis consists of endometrial tissue (the tissue that lines the inside of the uterus) growing outside the uterus is a common misconception. This view has been widely held due to the similar appearance and behavior of endometriosis lesions to endometrial tissue, including their response to hormonal changes throughout the menstrual cycle. Even Yale Medicine’s fact sheet on endometriosis notes that “Endometriosis occurs when the normal lining of the uterus starts to grow outside the uterine wall.” However, research has shown that the tissue found in endometriosis lesions is not identical to the endometrial tissue.
Endometriosis lesions are made up of tissue that is similar to, but distinct from, the endometrium. These lesions can bleed, thicken, and break down in a cycle similar to the menstrual cycle, leading to inflammation, pain, and the formation of scar tissue. Unlike the endometrium, which is shed from the body during menstruation, the tissue from endometriosis lesions has no way to exit the body, which can cause significant pain and other symptoms.
The exact origin of endometriosis tissue remains a subject of ongoing research and debate. Several theories exist, including retrograde menstruation (where menstrual blood flows back through the fallopian tubes into the pelvic cavity instead of leaving the body), metaplasia (where cells in the pelvic and abdominal lining transform into endometriosis-like cells), and embryonic cell transformation (where embryonic cells develop into endometriosis lesions under certain conditions).
The retrograde menstruation theory is still touted by many doctors but has been the subject of much endometriosis research and is often debated. After all, this study and others note that “Retrograde menstruation occurs in 76%–90% of women with patent fallopian tubes and not all of these women have endometriosis.” Much more research funding and more comprehensive medical education for women’s health professionals is needed before we fully understand the complexities of endometriosis.
Understanding that endometriosis involves tissue that is similar to but fundamentally different from endometrial tissue is crucial for accurate diagnosis and treatment of this painful disease. This distinction helps clarify why endometriosis is a complex condition requiring tailored and often multimodal treatment strategies, rather than being a simple extension of normal menstrual processes.
#10 Endometriosis Can Be Cured with Laparoscopic Surgery
The misconception that laparoscopic surgery to remove endometriosis lesions will cure the condition and put an end to debilitating pain associated with endometriosis is widespread but misleading. While laparoscopic surgery is one of several treatment options for managing symptoms of endometriosis (like chronic pain) and improving fertility in some cases, it is not a guaranteed cure for the disease.
Laparoscopic surgery, a minimally invasive procedure, allows doctors to remove or destroy lesions. Although surgery can provide some pain relief and improve quality of life, the nature of endometriosis means that there is a risk of recurrence. Even after surgical removal of endometriosis lesions, new lesions can form, and symptoms may return. Studies show variable recurrence rates, but there is a significant risk of symptoms returning within five years after surgery.
Microscopic lesions or deeply infiltrating endometriosis may not be visible or accessible during surgery, meaning not all endometriosis tissue can be removed. This residual tissue can continue to cause symptoms. Surgery addresses the physical manifestations of endometriosis but does not tackle the underlying causes of the disease, which are not fully understood but are thought to involve genetic, immune, and hormonal factors.
Many individuals may need ongoing treatment with hormonal therapies or other medications after surgery to manage symptoms and reduce the likelihood of recurrence. Women respond differently to surgery. While some may experience significant and long-lasting relief from symptoms, others may notice only a temporary improvement or minimal change in their symptoms.
Ways Some Women Lessen Symptoms of Endometriosis


Women living with endometriosis often explore various strategies to manage and lessen their symptoms. Many women combine lifestyle changes with medical treatments to lessen pain and limit inflammation. Since endometriosis can affect individuals differently, what works well for one person may not work for another.
Diet and Nutrition
Dietary adjustments can play a crucial role in managing endometriosis symptoms. An Anti-inflammatory Diet focuses on reducing intake of foods that might promote inflammation (such as gluten, red meat, dairy, and processed foods) while emphasizing fruits, vegetables, and omega-3 fatty acids, known for their anti-inflammatory properties.
The Low FODMAP Diet might be beneficial for those experiencing gastrointestinal symptoms alongside endometriosis. This diet helps identify and eliminate foods that are difficult to digest and may cause bloating, gas, and abdominal pain. It’s important to understand that digestive issues occur for many different reasons at various stages of digestion. As such, this type of diet might not be suitable for all women living with endometriosis.
Physical Therapy
Pelvic Floor Physical Therapy addresses pelvic pain associated with endometriosis by targeting muscle tightness and dysfunction in the pelvic floor. Through tailored exercises and techniques, physical therapy can help alleviate pain, improve muscular function, and enhance pelvic health, offering a non-invasive option for symptom relief.
Medical Treatments
Medical treatments are fundamental in managing endometriosis symptoms. Hormonal Therapies such as birth control pills, progestins, and GnRH (Gonadotropin-Releasing Hormone) agonists work by regulating hormone levels, which can suppress the growth of endometrial-like tissue and reduce pain.
Pain Medication, including nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen, is commonly used to alleviate menstrual cramps and pelvic pain. Of course, there are issues associated with long-term regular use of NSAIDs.
For those with severe symptoms or endometrial-like tissue that causes significant discomfort or fertility issues, Surgery might be considered. Laparoscopy, a minimally invasive surgical technique, allows for the removal of endometrial lesions with fewer complications and shorter recovery times compared to open surgery.
For those seeking or requiring Hormone-Free Medical Options, discussing non-hormonal pain management strategies and surgical alternatives with healthcare providers is essential. These options are particularly relevant for individuals who cannot use hormonal treatments due to side effects or other health considerations.
Finding a care team that has first-hand experience with endometriosis can help. For example, Dr. Alexis Gonzales, ND, IFMCP helps women with endometriosis adopt a functional medicine approach to endometriosis management. She lives with endometriosis personally.
Stress Reduction Techniques
Since stress can exacerbate endometriosis symptoms, incorporating Stress Reduction Techniques like yoga, meditation, and mindfulness into daily routines can be beneficial. These practices help manage stress, reduce pain perception, and improve overall emotional well-being, making them valuable tools in the comprehensive management of endometriosis.
Exercise
While chronic pain can make it feel impossible, Regular Exercise is important for managing endometriosis symptoms, improving physical health, and enhancing psychological well-being. Activities should be selected based on personal comfort and symptom response, with some women finding relief through low-impact exercises such as walking, swimming, or yoga, which can reduce pain and improve quality of life.
Alternative Therapies
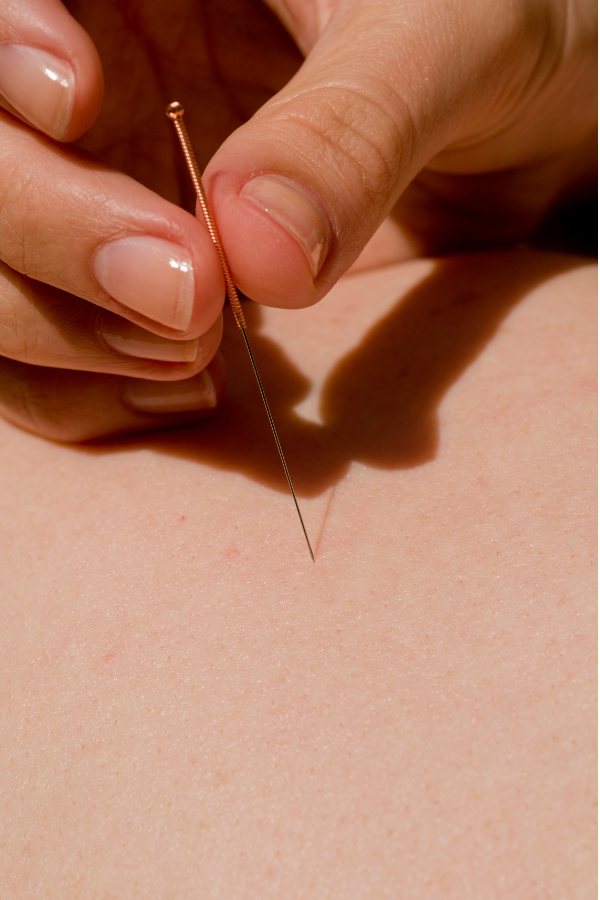
Alternative Therapies, including acupuncture, chiropractic care, and herbal supplements, are explored by some women as complementary treatments. These therapies may offer pain relief and help manage symptoms, but it’s crucial to discuss them with a healthcare provider to ensure they’re appropriate and safe, considering individual health needs and conventional treatment plans.
Support Networks
Support Networks play a vital role in coping with endometriosis. Joining support groups, whether online or in-person, offers emotional support, understanding, and shared experiences. These communities provide valuable insights and information, helping individuals navigate the challenges of living with endometriosis and fostering a sense of belonging.
Heat Therapy
Heat Therapy involves applying heat to the pelvic area, which can be achieved through heating pads, warm baths, or heat wraps. This simple yet effective method helps relax pelvic muscles, reduce cramping, and alleviate pain, offering immediate and non-invasive symptom relief.
Supplements
Certain Supplements, such as magnesium, omega-3 fatty acids, and vitamin B-complex, may help manage endometriosis symptoms by reducing inflammation, pain, and supporting overall health. It’s important to consult with a healthcare provider before starting any supplements to ensure they are suitable for your specific health situation and do not interact with other treatments.
Resources for Women Living with Endometriosis
For women living with endometriosis, finding reliable resources for information, support, and treatment options is crucial. Here are some valuable resources that can help.
Endometriosis Associations, Foundations, and Educational Resources
- Endometriosis Foundation of America (EndoFound): Offers educational resources, support, information about new treatments, and research updates on endometriosis.
- The World Endometriosis Society (WES): Provides information on global initiatives and research related to endometriosis.
- Endometriosis.org: A global platform for news, scientific developments, and community support related to endometriosis.
Healthcare Provider Directories
Finding a healthcare provider or a specialist who understands endometriosis can be challenging. Some organizations, like the Endometriosis Foundation of America, offer directories of endometriosis specialists. When seeking resources, it’s important to look for those that offer evidence-based information and support.
Consulting with healthcare professionals for personalized advice and treatment plans is also crucial. These resources can provide a starting point for education, support, and advocacy as you navigate life with endometriosis.
Online Forums and Support Groups


- Endometriosis UK: Offers a wide range of resources including information on managing endometriosis, support group meetings, and an online community.
- Online communities like Reddit (r/Endo and r/endometriosis) and HealthUnlocked Endometriosis community offer spaces for sharing experiences, advice, and support.
Research and Clinical Trials
- ClinicalTrials.gov: Provides a database of clinical studies worldwide, allowing you to search for ongoing endometriosis research and trials.
Books and Literature
There are several informative books on endometriosis that offer insights into managing the disease, understanding its symptoms, and exploring treatment options. Titles include “Heal Endo: An Anti-Inflammatory Approach to Healing from Endometriosis” by Katie Edmonds, “Endometriosis: A Key to Healing Through Nutrition” by Dian Shepperson Mills and Michael Vernon, and “The Doctor Will See You Now: Recognizing and Treating Endometriosis” by Tamer Seckin, MD.
Bear in mind that nearly all books about endometriosis include some controversial or poorly researched information about the condition. We hope that awareness contributes to more ongoing research, as there is only so much information available about the origins and treatment of endometriosis.
Editor’s Note to Readers


Endometriosis is frustrating for many and can be heart-breaking for some. But each day, we learn more about the condition and the ways in which our individual bodies react to different treatments, lifestyle alterations, diets, and other types of support.
None of us is alone in this, and while we might fear the pity, frustration, or ignorance of others, most of the people who love us are inspired by how we continue to search for ways to improve lives lived with endometriosis. And there is hope to support this ongoing search. New research studies and clinical trials are published every year, alternative medicine is increasingly accepted and respected, and there’s an enormous community available to us online.
At DesignDash, we hope you give yourselves a little extra grace this Endometriosis Awareness Month. We’ll be thinking of you! And if you love someone with this condition, consider sending a bouquet of flowers and a sweet note this month. A little bit of understanding goes a long way.








