Medical Gaslighting: What it is, How it Impacts Women, and Why it Hurts So Much
Summary
Reflection Questions
Journal Prompt
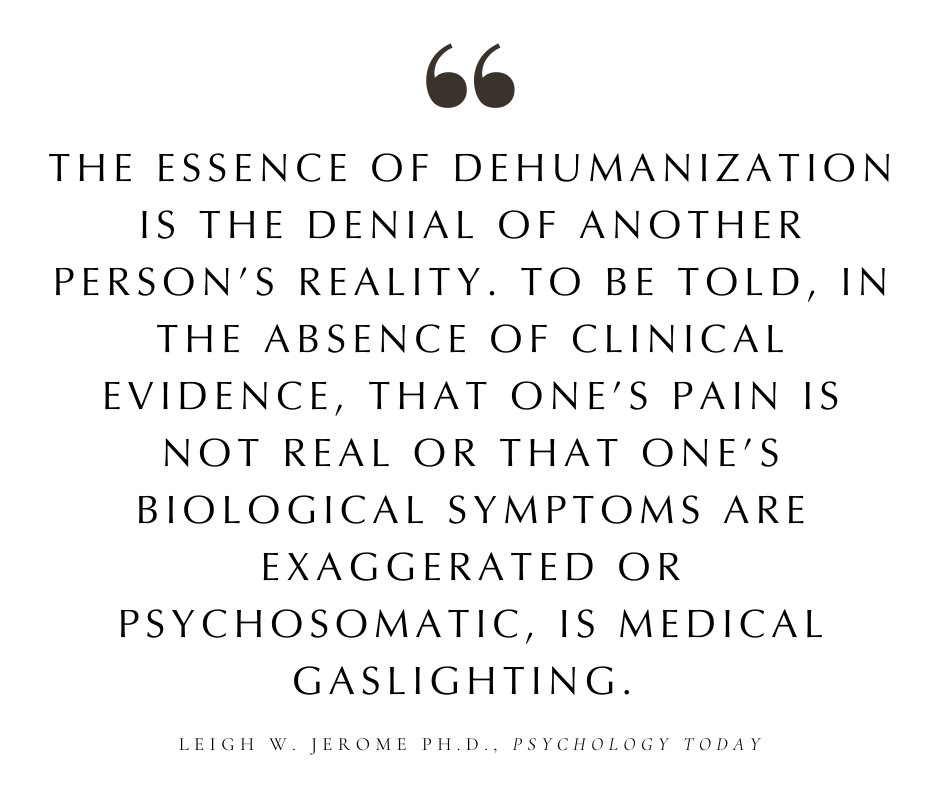
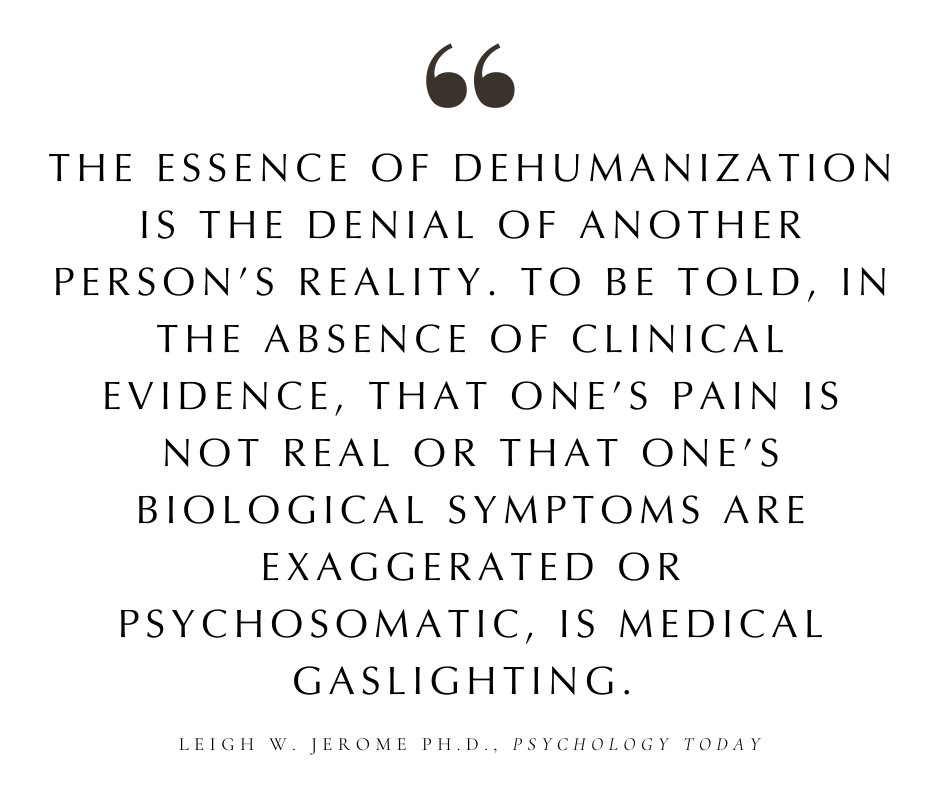
Medical gaslighting, a term that is gaining increasing attention within the healthcare sector, refers to the phenomenon where patients’ symptoms and concerns are dismissed or minimized by healthcare professionals, leading to misdiagnosis, poor clinical decision making, delayed treatment, or no treatment at all. These cognitive biases are particularly insidious when they intersect with gender and race, notably impacting women, and even more profoundly affecting women of color. Women, who have historically been subjected to biases and stereotypes in various spheres of life, find these prejudices magnified within the medical context, where their health concerns are often not taken as seriously as those of their male counterparts.
For women of color, the intersectionality of gender and racial biases compounds the challenge, leaving them disproportionately vulnerable to the consequences of medical gaslighting. The importance of addressing medical gaslighting cannot be overstated, as it not only undermines the trust essential for effective patient-provider relationships but also perpetuates systemic inequities within healthcare. In this article, we will explore the health prevalence of this cognitive bias in health care, delve into its psychological and physical repercussions, and advocate for systemic changes needed to combat this pervasive issue. We aspire to contribute to a more equitable system in which health care professionals recognize and addresses the unique challenges faced by women, thereby improving health outcomes and patient safety for all.
Understanding Medical Gaslighting
The term “gaslighting” originates from the 1938 stage play “Gas Light,” where a husband manipulates his wife into questioning her reality to conceal his wrongdoings. This psychological manipulation has since been recognized in various contexts, including healthcare, where it is known as medical gaslighting.
In the medical industry, gaslighting occurs when healthcare professionals dismiss or trivialize patients’ symptoms, leading them to doubt their own experiences. This transition from a broad psychological concept to a specific medical issue highlights the complex dynamics between patients and healthcare providers, underscoring the need for a deeper understanding and acknowledgment of patients’ concerns and symptoms.
How it Manifests in Healthcare
Medical gaslighting manifests in healthcare through a variety of scenarios, each potentially devastating to the patient’s well-being. Common examples include a doctor suggesting a patient’s severe pain is just stress, or attributing palpable symptoms to anxiety without thorough investigation. Such dismissals can delay diagnoses, exacerbate conditions, and deeply impact patients’ mental health.
The dynamics between patients and practitioners are central to these scenarios. Power imbalances, where patients feel their voices are less valued or heard, play a significant role. This dynamic is particularly problematic when it intersects with gender, race, and socioeconomic status, further complicating the patient’s ability to be taken seriously and receive desired health care outcomes.
Biases in the Healthcare System
Bias in the healthcare system (i.e., confirmation bias, implicit bias, weight bias, etc.) is directly responsible for much medical gaslighting. Cognitive bias refers to systematic cognitive errors in thinking that affect decisions and judgments. In the context of healthcare, these biases can lead healthcare providers to form quick judgments based on their personal experiences, beliefs, or limited information rather than on a comprehensive evaluation of the patient’s symptoms and medical history.
For instance, a doctor might dismiss a patient’s symptoms as anxiety or stress without thorough investigation, due to a cognitive bias known as diagnostic overshadowing, where a perceived primary diagnosis overshadows actual, underlying conditions. This kind of bias contributes to medical gaslighting by dismissing or diminishing the patient’s experience and concerns without due diligence.
Implicit Bias and Its Impact


Implicit bias involves attitudes or stereotypes that affect our understanding, actions, and decisions in an unconscious manner. These biases are particularly detrimental in healthcare settings, as they can lead to unequal treatment of patients based on race, gender, age, or weight. Women, especially women of color, are disproportionately affected by implicit biases. Such biases have led certain institutions to issue the Implicit Association Test to cut down on health care disparities related to weight, gender, and racial bias.
Studies have shown that medical professionals may unconsciously perceive women and particularly women of color as being more prone to overreacting or being less credible about their symptoms. This bias not only undermines the patient-doctor relationship but also contributes to the gaslighting experience, as the implicit attitudes and stereotypes held by healthcare providers can lead them to dismiss or underestimate the patients’ concerns.
Weight bias in healthcare is another significant factor that contributes to medical gaslighting. It refers to the negative attitudes, beliefs, and judgments about individuals based solely on their weight or body size. This form of bias can deeply affect the quality of healthcare that overweight or obese patients receive, leading to instances of medical gaslighting that can have serious repercussions for a patient’s health and well-being.
Healthcare professionals may hold conscious or unconscious biases that overweight or obese individuals are non-compliant, lack willpower, or are responsible for their health issues. This bias can lead to quick, unfounded judgments about a patient’s symptoms, attributing them to weight without a thorough investigation or consideration of other possible causes. As a result, patients may be told that all their health issues would improve if they just lost weight, without receiving appropriate diagnostic tests or referrals that would address their actual medical concerns. This dismissive approach not only undermines the patient’s experience and concerns but can also delay proper diagnosis and treatment.
The Prevalence of Medical Gaslighting
The prevalence of medical gaslighting, though challenging to quantify precisely due to its nuanced and subjective nature, has been increasingly recognized in patient-reported experiences and some clinical studies. Surveys indicate a significant portion of patients feel their concerns have been dismissed or minimized by healthcare professionals, with women and individuals from marginalized communities reporting higher rates of such experiences.
The demographic breakdown reveals that medical gaslighting disproportionately affects women, especially women of color, who report higher instances of being ignored or misunderstood by medical practitioners. These health disparities suggests a complex interplay of gender and ethnicity biases in the healthcare system, underscoring the need for further research and a systematic review of the data to understand the full scope of the issue.
For example, specific conditions like endometriosis, which predominantly affects individuals assigned female at birth, can take an alarmingly long time to diagnose—seven to ten years on average. This delay is partly due to the normalization of menstrual pain and the assumption that extreme discomfort is a typical aspect of menstruation, illustrating how gender biases can lead to inadequate healthcare responses. According to this article published in Psychology Today, women are also more likely than men to receive a mental health diagnosis instead of proper treatment for their physical symptoms, facing longer wait times for diagnoses of serious conditions like cancer or heart disease.
Other Areas in Which Women Suffer From Medical Gaslighting and Inconsistent Understanding of Women’s Bodies


Cardiovascular Diseases: Studies have shown that women are often underdiagnosed and undertreated for cardiovascular diseases compared to men. Women’s symptoms are sometimes less recognized as being related to heart disease, leading to delays in treatment.
Mental Health: Women are more likely to be diagnosed with anxiety and depression, and their mental health conditions are often treated differently than men’s. This can affect the outcomes and effectiveness of the treatment.
Autoimmune Diseases: Women are more prone to autoimmune diseases than men, but the recognition and diagnosis of these conditions can be challenging, leading to delays in treatment and disparities in outcomes.
Pain Management: Research has indicated that women’s pain is often taken less seriously than men’s, leading to disparities in the management and treatment of pain.
Cancer Diagnosis and Treatment: Certain cancers, such as lung and colorectal cancer, show differences in survival rates between men and women, influenced by factors like stage at diagnosis, treatment options offered, and biological differences.
Reproductive Health: Women’s reproductive health issues, including pregnancy-related conditions, are areas where disparities can be particularly pronounced, affecting both maternal and infant health outcomes.
Reporting and Documentation Challenges
The issues surrounding the underreporting and inadequate documentation of medical gaslighting are significant barriers to grasping its prevalence and impact. Many patients who experience gaslighting may not report these incidents due to feelings of shame, fear of not being believed, or lack of awareness that their experiences constitute gaslighting.
Additionally, the subjective nature of gaslighting makes it difficult to document and quantify in medical records, leading to a lack of concrete data. Healthcare systems often lack standardized protocols for patients to report dismissive or minimizing behavior, contributing to the invisibility of the problem and additional diagnostic errors. These challenges highlight the need for improved mechanisms within healthcare settings to encourage reporting and documentation, ensuring that instances of medical gaslighting are recognized and addressed.
Physical and Psychological Repercussions of Gender Bias and Gaslighting in Clinical Medicine


The disparities in healthcare between women and men can lead to significant psychological and physical repercussions. For women, these disparities often manifest as less recognition of their symptoms and a delay in receiving accurate diagnoses and effective treatments. This neglect not only exacerbates their current health condition but can also lead to additional stress and anxiety, compounding the physical toll on their bodies. Men, on the other hand, might face challenges in receiving adequate care for mental health issues or conditions perceived as less masculine, affecting their overall well-being. This is why bias awareness amongst health care professionals is so vital.
Short-term Effects
In the short term, these disparities can cause significant emotional distress and foster mistrust in healthcare providers. When individuals feel their concerns are minimized or dismissed, it not only affects their current health situation but also their confidence in seeking medical help. This emotional turmoil can lead to heightened stress, which is known to have adverse effects on physical health, including increased blood pressure and a weakened immune system, setting the stage for further health complications.
Emotional Distress and Mistrust in Healthcare Providers


Emotional distress stemming from healthcare disparities can deeply affect one’s mental health, leading to feelings of frustration, sadness, and anger. When patients perceive that their health concerns are not taken seriously or are misdiagnosed based on gender biases, it can lead to a profound mistrust in healthcare providers. This mistrust can discourage individuals from sharing important symptoms or health concerns in future consultations, potentially leading to missed or delayed diagnoses.
Long-term Consequences
Over time, these disparities can result in chronic health issues and the worsening of existing conditions. The cumulative effect of delayed diagnoses, inadequate treatment, and lack of follow-up care means that manageable conditions can become severe, leading to decreased quality of life and increased mortality rates. For example, cardiovascular diseases may progress further in women before they are correctly diagnosed and treated, directly impacting their long-term health outcomes.
Chronic Health Issues and Worsening Conditions
The long-term neglect of gender-specific healthcare needs can exacerbate chronic conditions and lead to the development of secondary health issues. For instance, untreated depression or anxiety can worsen cardiovascular health, while poorly managed pain can lead to chronic pain syndromes, further diminishing life quality and increasing healthcare costs over time.
Impact on Healthcare-seeking Behavior
The experiences of being undervalued or misunderstood by healthcare providers can significantly impact individuals’ healthcare-seeking behavior. Many may choose to avoid or delay seeking treatment for future health issues, fearing further dismissal or misunderstanding. This avoidance behavior can be particularly detrimental, as early detection and treatment of many conditions can drastically improve outcomes and prevent complications.
Avoidance and Delayed Treatment


The avoidance of healthcare services and delayed treatment initiation are direct consequences of negative healthcare experiences. This behavior not only puts individuals at risk of late-stage diagnoses when diseases are more difficult to manage but also increases the likelihood of emergency situations, which could have been prevented with timely care. The cycle of avoidance and delayed treatment perpetuates the disparities in health outcomes between genders, underlining the need for a more inclusive and empathetic healthcare approach.
Combating Medical Gaslighting
Medical gaslighting, where patients’ symptoms are dismissed or downplayed by healthcare providers, has significant implications for patient outcomes and trust in the healthcare system. Addressing this issue requires a multifaceted approach, focusing on empowering patients, educating healthcare professionals, and implementing policy and systemic changes.
Empowering Patients
Empowering patients involves teaching strategies for self-advocacy and effective communication with healthcare providers. This can include preparing detailed accounts of symptoms, maintaining a health diary, and being assertive about concerns. It’s also beneficial for patients to seek a second opinion when they feel their concerns are not being adequately addressed. Providing resources and support groups can also help patients feel more confident in navigating the healthcare system and advocating for their health needs.
Educating Healthcare Professionals
Educating healthcare professionals is crucial to combat medical gaslighting. Training programs that focus on recognizing unconscious biases, practicing empathy, and delivering patient-centered care can make a significant difference. By understanding the diverse ways in which conditions can present and acknowledging the validity of patients’ experiences, healthcare providers can improve diagnostic accuracy and patient trust. Continuing education on the importance of listening to and validating patient concerns is vital for fostering a more inclusive and respectful healthcare environment.
Policy and Systemic Changes
Policy and systemic changes are necessary to create a healthcare environment where medical gaslighting is actively discouraged. This includes initiatives for accountability, such as patient feedback systems, and reform policies that ensure equitable care for all patients.
Healthcare institutions should implement standards for patient care that emphasize the importance of listening to and respecting patient narratives by health professionals. Moreover, policies that support the integration of patient advocates into the healthcare team can help bridge communication gaps between patients and providers, ensuring that all patients feel heard and valued.
Combating medical gaslighting requires concerted efforts from individuals, healthcare professionals, and policymakers. By empowering patients, educating healthcare providers, and enacting systemic changes, we can create a more equitable and compassionate healthcare system.
Resources for Women Seeking Better Representation After Experiencing Medical Gaslighting


For women, particularly women of color, who feel gaslighted or dismissed in healthcare settings, finding supportive resources and communities can be crucial for navigating these challenges. Here are some valuable resources aimed at empowering women and advocating for their health:
National Organizations and Websites
Black Women’s Health Imperative – This organization focuses on addressing the health disparities faced by Black women. They provide resources, advocacy, and health information to empower Black women to advocate for their health. Go to bwhi.org for more information.
The National Women’s Health Network (NWHN) – NWHN advocates for women’s health by influencing policy and supporting women in making informed health decisions. They offer resources on a wide range of health topics and actively work to end medical gaslighting. Go to nwhn.org for more information.
Asian & Pacific Islander American Health Forum (APIAHF) – This organization focuses on improving the health of Asian Americans, Native Hawaiians, and Pacific Islanders. They provide resources and advocate for policies that address healthcare disparities. Go to apiahf.org for more information.
National Latina Health Network (NLHN) – NLHN addresses the health needs of Latina women by advocating for healthcare access, quality, and equity. They provide education and resources to empower Latina women in their healthcare journeys. Go to nlhn.net for more information.
Online Forums and Support Groups
PatientsLikeMe and HealtheVoices are platforms where individuals can share their healthcare experiences and find community support. Women can find others who have faced similar challenges, including experiences of being gaslighted in healthcare settings.
Advocacy and Legal Resources
The Center for Patient Partnerships – This organization offers advocacy and support for patients navigating the healthcare system, providing resources to empower individuals in advocating for their healthcare needs. Go to patientpartnerships.org for more information.
The American Civil Liberties Union (ACLU) – The ACLU works on issues of discrimination in healthcare and can be a resource for legal support if a woman feels her rights have been violated. Go to aclu.org for more information.
Educational Resources
Speaking Up About Care – Various health organizations provide guidelines and tips for advocating for oneself in medical settings. Materials on how to effectively communicate with healthcare providers, prepare for appointments, and seek second opinions can be empowering.
Apps and Tools
MyHealthTeams – This social network for chronic conditions has specific communities where women can share experiences and support each other, including navigating instances of gaslighting in healthcare.
Books
“Doing Harm: The Truth About How Bad Medicine and Lazy Science Leave Women Dismissed, Misdiagnosed, and Sick” by Maya Dusenbery – This book delves into the systemic issues leading to women being dismissed in healthcare and offers insights on advocating for oneself.
Empowerment and advocacy begin with being informed and connected. These resources can provide women, especially women of color, with the support and tools needed to navigate the healthcare system more effectively and to advocate for the care and respect they deserve.








